The challenge of recruiting suitable patients into clinical trials has always been a significant obstacle to drug and medical device development programs. The difficulty of generating evidence delays the introduction of new medical interventions and results in high costs. In a new Covid-19 environment, the pharmaceutical industry is facing unprecedented pressures. As the global population of people with multiple chronic diseases increases (now estimated at one in three adults), the need and urgency to address the challenges of enrollment and effective engagement of patient cohorts is a critical issue for the evolution of medical care.
A key goal is to address research and development cost structures and improve the efficiency and effectiveness of the clinical development process. Improving patient recruitment, involvement, and retention is an essential component. The pharmaceutical industry is at the center of a digital revolution that has the potential to transform the healthcare ecosystem.
By implementing strategies focused on the patient pathway, trial centers may be able to implement a simpler model of care. New technologies, such as Digital Health platforms and social media, are designed precisely to help patients connect with physicians so that they can more easily and quickly access information and services according to innovative and sustainable models of care.
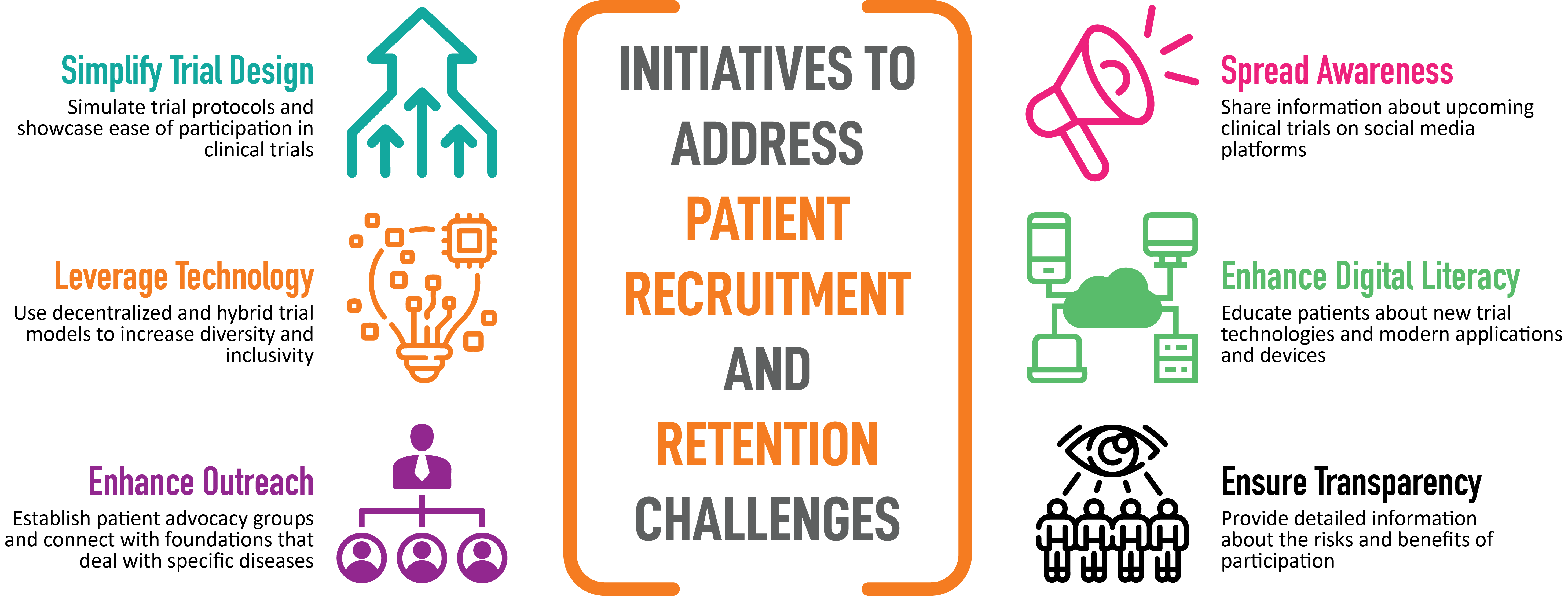
STRATEGIES FOR PATIENT RECRUITMENT AND RETENTION
The best recruitment and retention strategies for clinical trials focus on the patient perspective. To be successful, a reliable program must be developed with the use of a variety of outreach and education methods designed to reach patients quickly and efficiently, providing them with the information they need for their treatment choices. This article examines the challenges faced and initiatives successfully implemented in recent studies.
REASEARCH CHALLENGES
Randomized controlled trials (RCTs) are widely accepted as the gold standard for evaluating new therapies. Recruitment is often slower or more difficult than expected, and many studies fail to reach the expected sample size within the time frame and with the funding dedicated to the study. If the target number of patients is not reached, the results will usually be less reliable. If the recruitment period has to be extended, costs usually increase and the application of results in clinical practice is delayed.
As an illustrative case in point, a multiple sclerosis study recently published in the journal JAMA was partially compromised by much slower recruitment than expected, necessitating a reduction in the number of patients enrolled (in accordance with the FDA regulatory agency). From a statistical point of view, this variation reduces the reliability of the results and requires specific analyses to analyze the bias introduced by differences in the number of patients enrolled, which was very low (<3 patients) in 30% of the centers involved.
Hospitals conducting clinical trials are often plagued by high staff turnover and limited by inefficient infrastructure. As a result, center staff are often overloaded and forced to prioritize multiple patient-facing tasks, resulting in a potential loss of study candidates and/or an increase in patients dropping out of the trial before its completion.
Of no less importance is the inconvenience to the patient represented by the burden that many studies entail, such as frequent visits, invasive procedures, and distances to travel to the center, so the patient is disincentivized from participation.
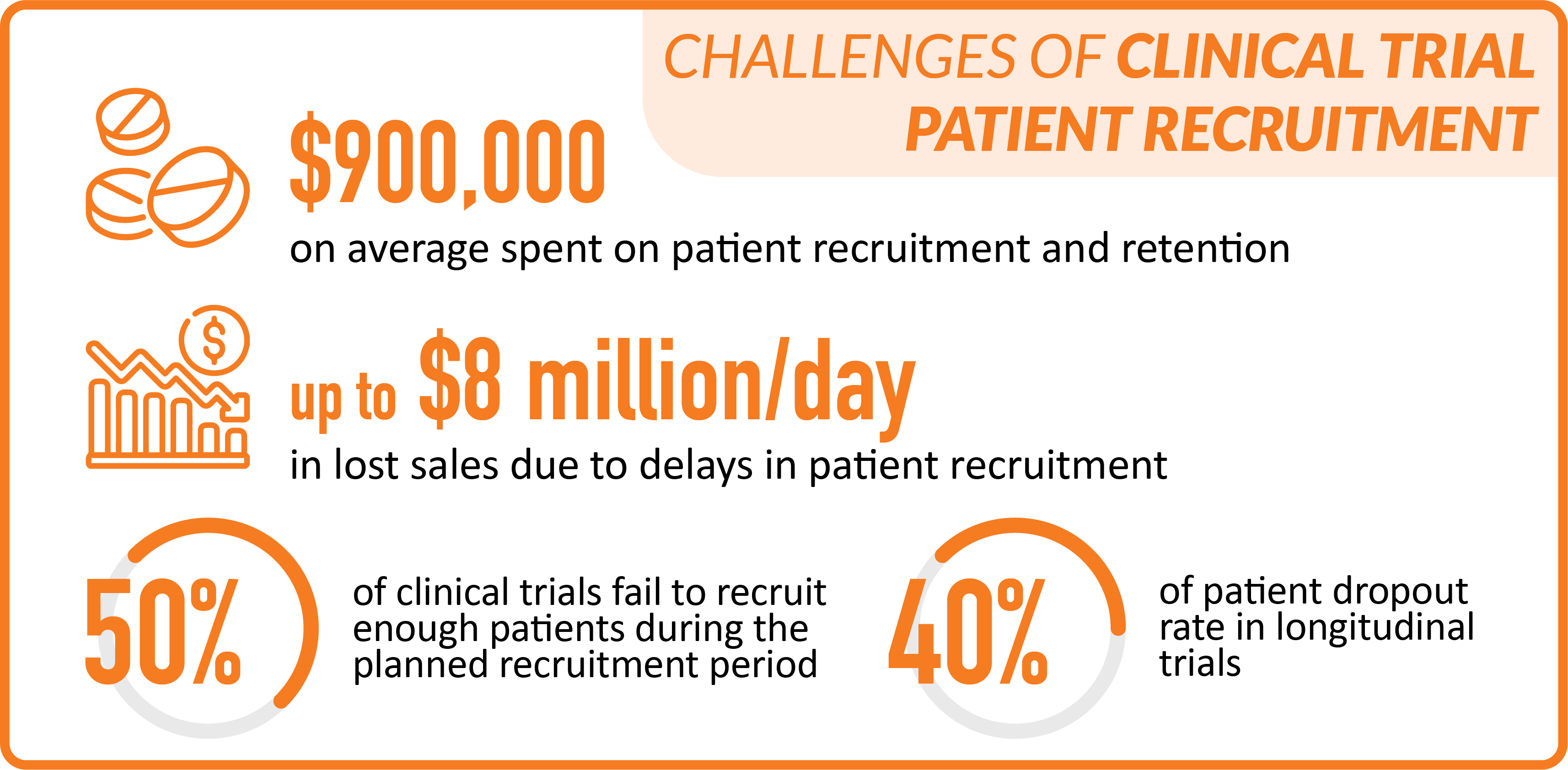
ECONOMIC IMPACT
Biopharmaceutical companies spend an average of nearly $900,000 on patient recruitment and adherence during new drug development. Despite this investment, nearly 50 percent of clinical trials fail to recruit enough subjects during the planned period. Delays in patient recruitment can cause the timing of commercialization to slip significantly, resulting in revenue losses that are estimated at up to $8 million per day in lost sales. These problems are compounded by patient dropout rates, which can be as high as 40 percent in longitudinal studies.
DECENTRALIZED STUDIES
Decentralized clinical trials (DCTs), in which clinical trial data are collected through sensors or remote monitoring devices carried by the patient without the need to visit a clinical center, can offer many benefits to pharmaceutical companies, including cost savings, better patient recruitment and retention, and improved data quality.
Before the Covid-19 pandemic, significant information existed on the benefits of DCTs, but only a few pilot projects used these technologies, as companies were disincentivized by regulatory uncertainties, the need for upfront investment in sensors and products, and the limited functionality of available technologies. Today, DCTs have proven to be a lifesaver for restarting clinical trials that were interrupted during the pandemic. Moreover, recent technological advances, the proliferation of wearable devices (wearables), and the FDA’s push to adopt DCTs after the Covid-19 case have made the DCT landscape ripe for a breakthrough.
The main advantage of decentralized clinical trials is the opportunity to improve the patient experience. But the remote model has reduced in-person interactions. Poor communication by sites and sponsors is often at the root of current challenges in recruiting and enrolling patients in clinical trials. The human touch, an important psychological aspect in health care, is lacking in this model. Added to this is the burden of learning about new products and technologies. All of these factors create a general sense of discomfort and disengagement among patients, creating additional problems for clinical trial acceptance. However, more recent studies, such as those described below, show how these barriers can be overcome.
THE SEARCH FOR THE FUTURE
A recent study has shown how decentralized trials, even large ones, can expand access to testing and reduce the risk of exposure for patients and staff. The DeTAP (Decentralized Trial in Afib Patients) study, conducted entirely during the Covid-19 pandemic, integrated a range of digital technologies, including paired home sensors, into a 100 percent virtual trial experience in atrial fibrillation (AF) patients on anticoagulation. The study recruited 100 participants in 26 days (traditional recruitment: 6 patients in 2 weeks; social media: 94 patients in 12 days). Moreover, over-recruitment occurred with more than 200 eligible candidates on the waiting list. All major study completion metrics showed high compliance: telemedicine visit (91%); patient questionnaires (85%); completion of ECG and sensor blood pressure measurement (90%). This demonstrated that a decentralized cardiovascular intervention study is feasible and can achieve rapid recruitment, high study retention, reporting of physiological events or adverse events, and high study involvement through proper integration of digital technologies and a DCT study coordination effort.
In the summer of 2021, the NIH (National Institute of Health), along with other U.S. government agencies, launched Operation Warp Speed. The goal was to accelerate the development, production, and distribution of medical countermeasures for Covid-19. Interested individuals signed up for a registry on a website, which had security protections. Clinical trial staff used the registry to contact and select potential study volunteers. The program achieved recruitment of 600,000 volunteers in the first 6 weeks, a group that represented a wide variety of demographics and enrolled in multiple Phase III studies of Covid-19.
These results indicate how virtualization of enrollment and conduct of large pivotal clinical trials at scale is now possible.
WEB AND SOCIAL MEDIA USE
In the United States in recent years, to accelerate recruitment, researchers have expanded traditional methods, such as newspaper, radio or television advertising, flyers and signage on buses, with social media strategies. In Europe, traditional methods for patient recruitment include flyers and posters distributed in hospitals and/or general practitioners’ offices. Materials can only be used after approval by the relevant ethics committee.
Social media can be a useful tool for patient recruitment because of its ability to target personalized messages to specific patients. In addition, several social media platforms have a higher percentage of users from minority groups (e.g., African American use of Twitter), facilitating enrollment of different ethnic groups.
The use of the web and social networks to recruit patients in recent years has grown tremendously in the United States, allowing the target population to be reached certainly more quickly than traditional recruitment methods: reaching patients on social media, for example, through the many groups in which patients share their experiences, united by a disease or therapy, allows them to interact with patients and provide information about the study.
INVOLVEMENT OF PHYSICIANS AND PATIENTS
Sending newsletters to participating centers and holding meetings with key players involved in clinical trials provide an excellent opportunity to share information and progress on enrollment-which is often competitive-at individual centers. This can be a stimulus for centers that are slower in enrollment. Organizing webinars and seminars between the various trial centers and patient associations to allow participating patients to take direct action on trial issues can increase the chances of enrollment, given the increasingly important role of patients in the success of clinical trials.
Involve physicians on the ground or in outpatient clinics, who are approached by patients in the first instance. GPs generally do not have the potential to enroll patients for clinical trials, but they care deeply about their patients and are willing to refer clinical trials when appropriate. To increase the likelihood of enrolling new patients in the clinical trial, it is useful to consider the relationship between the patient and the general practitioner; simple and concise communication to the physician, using digital engagement systems, allows them to convey salient but comprehensive information about the trial, track the reading, and plan subsequent communications based on the results obtained in terms of contact with potential new patients.
HOW TO APPLY THE NEW MODELS
In order to provide a superior patient experience and take full advantage of new technologies and models for conducting trials, companies and study stakeholders need to be aware of clinical trial enrollment challenges that could be major obstacles. A deeper analysis of the major challenges, specific to each study, is critical for companies to develop effective measures for patient engagement and retention.






Leave A Comment